High blood pressure can rapidly transform healthy arterial cells into inflammation-prone “foam cells” that pose an increased risk of cardiovascular-related issues.
Scientists have recently revealed in a new study that high blood pressure has the potential to convert healthy arterial cells, known as vascular smooth muscle cells, into fatty “foam cells” that are susceptible to inflammation and cell death.
“It was especially surprising how quick the cells respond to the pressure and started forming [fatty] droplets within just a few minutes,” explained Thomas Iskratsch, professor of cardiovascular mechanobiology and bioengineering at Queen Mary University London and the study’s corresponding author.
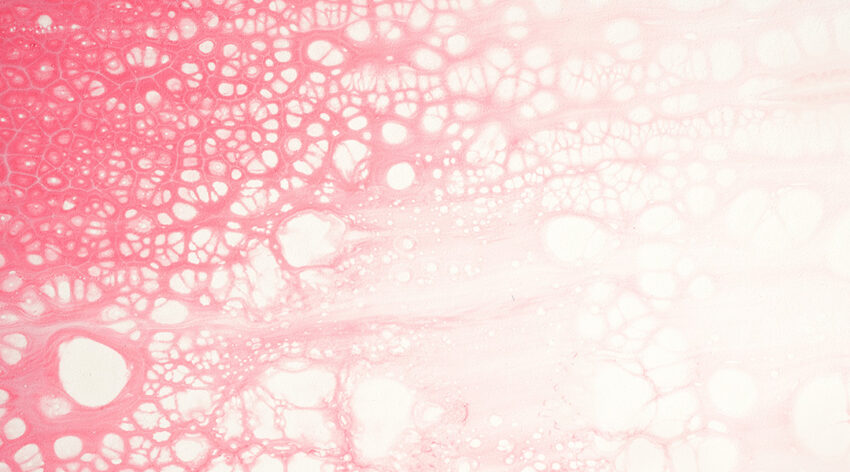
Vascular smooth muscle cells are the most common cells found in a healthy artery wall, and contract to help push blood through the body. But autopsies done in the 1980s began to suggest that these cells had begun accumulating cholesterol, transforming into an excessive amount of foam cells — a type of cell that removes fats or lipids from their environment.
“Taking up the lipids gives them the foamy appearance,” explained Iskratsch. “This type of behavior is typically associated with macrophages, a type of white blood cells. [Recently,] vascular smooth muscle cell-derived foam cells have come into focus and it appears now that they make up half of all foam cells, or more in the atherosclerotic plaque [a fatty material that builds up inside your arteries].”
Left unaddressed, these changes contribute to the thickening or hardening of arterial walls, increasing the risk of heart failure, stroke, or kidney damage. Despite previous research identifying signaling pathways responsible for the shift from healthy vascular cells to foam cells, the specific initiators and how they form has remained unknown. Iskratsch and his team therefore aimed to unravel the underlying forces causing this transition.
“[A previous study of ours] showed that smooth muscle cells respond to different mechanical stimuli i.e., stretching, stiffer environment, high hydrodynamic pressure, progressing into [disease],” said the study’s first author, Pamela Swiatlowska. The next step, she said, was to connect the dots using bioinformatic analysis, the application of computational and statistical techniques to extract meaningful information from their biological data, combined with cell and molecular biology experiments. The results led to a range of experiments that uncovered the mechanism of foam cell formation.
Cells have the ability to sense their environments, a crucial aspect of their survival and functioning as it allows them to respond to changes and adapt. Stiffness as a result of increased pressure has been implicated in a range of different diseases, and in their paper published in Advanced Science, Iskratsch, Swiatlowska, and their co-workers demonstrated for the first time how a molecule called Piezo1, which is sensitive to changes in mechanical forces, induced the switching to a foam cell type.
To do this, the team used an imaging technique called hyperspectral stimulated Raman scattering to help map different biomolecules within specific cellular compartments like the nucleus or cell membrane. This method combines Raman spectroscopy principles — where light scattering reveals information about chemical groups, aiding identification through unique patterns — with hyperspectral imaging, offering detailed data for various points in a sample and facilitating the mapping and identification of different molecules within the cells.
They demonstrated that the lipid droplets formed quickly when pressure stimulation and Piezo1 activation occurred. This suggests a direct mechanism, not one involving gene regulation as was previously proposed.
“Our work unlocks new avenues in atherosclerosis treatment,” said Swiatlowska. “We hope that by targeting mechanosignaling pathways, we’ll be able to develop new therapeutic strategies.”
“The findings could be also applicable to other organ systems and diseases,” added Iskratsch. “Hydrostatic pressure for instance increases in malignant solid tumors. Lipid droplets have been observed in a range of different tumors, where they are linked to tumor progression, so it would be interesting to study if similar pathways are at play. Likewise, Piezo1-dependent mechanosensing has been also linked to fat cell maturation and the pathways described in our work could be potential targets to [treat] obesity.”
Reference: Pamela Swiatlowska, Thomas Iskratsch, et al., Hypertensive Pressure Mechanosensing Alone Triggers Lipid Droplet Accumulation and Transdifferentiation of Vascular Smooth Muscle Cells to Foam Cells, Advanced Science (2023). DOI: 10.1002/advs.202308686