Scientists are making strides toward a potential new treatment for diabetic limb ischemia, a common and serious complication of diabetes. This condition, marked by reduced blood flow to the legs and feet, can result in chronic pain, stubborn ulcers, and, in severe cases, limb amputation — and is currently the leading cause of non-traumatic amputations.
People with diabetic limb ischemia also face significantly higher risks compared to those with other artery diseases, such as a 20%–30% greater chance of cardiovascular events and an alarming 14 times higher likelihood of amputation.
“Our primary motivation is to find a safer, non-surgical option for diabetic limb ischemia patients who often suffer from restricted blood flow and tissue damage in the lower limbs,” said Xing Zhang, a researcher in the Department of Vascular Surgery, Shanghai Ninth People’s Hospital in China and one of the contributing scientists on the study published in Advanced Healthcare Materials. “Current treatments, like surgery or medication, have risks and may not always be effective.”
Zhang and his team have spent the past decade working on stem cell therapies for vascular diseases. However, they encountered challenges, including immune rejection, tumor risks, ethical concerns, and unstable cell survival rates.
They needed an alternative.
Extracellular vesicles
An emerging therapy is based on extracellular vesicles, which are lipid bound particles that carry biomolecules and are naturally released from almost all types of cells. “Extracellular vesicle transplantation, particularly exosome transplantation, offers several advantages over traditional stem cell transplantation,” wrote the team in their paper, as they overcome all the barriers posed by stem cell therapy.
A critical step in extracellular vesicle therapy is identifying a protein or gene that can guide the vesicles and enhance their effectiveness for treating the target disease because these proteins or genes help direct the vesicles to the specific cells or tissues that need treatment.
By modifying or selecting proteins that target certain receptors or pathways, scientists can ensure that the vesicles deliver their cargo—such as therapeutic molecules or genetic material — precisely where it is needed. This targeting is essential for maximizing the therapy’s effectiveness and minimizing potential side effects or unwanted interactions with off-target tissues.
Previous studies have demonstrated that Netrin1, a protein known for its protective role in the cardiovascular system, can promote blood vessel growth, support cell survival, and reduce inflammation — all detrimental factors associated with diabetic limb ischemia.
“Netrin1 has primarily been studied for its role in nervous system development, especially in guiding nerve cells,” explained Xinwu Lu, director of the Department of Vascular Surgery at Shanghai Ninth People’s Hospital. “It hasn’t been commonly linked to conditions like diabetic limb ischemia, which involves complex issues like restricted blood flow, immune responses, and inflammation.”
However, its specific role in diabetic limb ischemia remains unclear, prompting the team to explore it as both a marker of and a potential therapeutic target for diabetic limb ischemia.
Promising first steps for diabetic limb ischemia
They began by investigating Netrin1 levels in blood and tissue samples collected from diabetic limb ischemia patients and used samples from acute arterial embolism patients as controls.
“Our results showed that Netrin1 levels were significantly lower in diabetic limb ischemia patients compared to controls,” explained Zhijue Xu, assistant researcher at Shanghai Jiao Tong University. “This finding suggests that reduced Netrin1 levels may play a role in [the disease’s] progression and encouraged us to look further into its therapeutic potential.”
The goal was to use genetically modified stem cells derived from fat tissue that produce higher levels of Netrin1. They do this by releasing exosomes — tiny, vesicle-like particles — that contain Netrin1 into their surrounding environment during their regular cellular processes.
“Exosomes were collected through a process called differential ultracentrifugation, which isolates and purifies them based on their size and density,” the team explained. “Once purified, these exosomes, enriched with Netrin1, were injected directly into ischemic tissues. There, they help improve blood flow and promote tissue repair, offering a potential therapeutic option for conditions like diabetic limb ischemia.”
Improving tissues’ healing capacity
The Netrin1-enriched exosomes were found to outperform regular adipose-derived stem cell exosomes in initial experiments. “This is because Netrin1 activates protective pathways within cells, helping them withstand stressful conditions,” said Yihong Jiang, postdoctoral researcher in Vascular Surgery at Shanghai Ninth People’s Hospital.
By combining Netrin1’s protective and blood vessel-promoting effects, Netrin1-enriched exosomes significantly improve the healing capacity of tissues affected by diabetic limb ischemia.
The key to its success was the activation of two cellular pathways involved in survival and repair. “One pathway encourages angiogenesis, improving blood flow to ischemic tissue, while the other speeds up cell growth and tissue repair,” said Jiang. “When activated by Netrin1-enriched exosomes, these pathways provide a kind of ‘protective shield’ for blood vessel cells, helping them recover and repair damaged tissues more quickly and effectively.”
Compared to invasive procedures like stent placement or bypass surgery, Netrin1-enriched exosomes offer a promising non-surgical option by helping cells naturally repair themselves and restore blood flow to the affected limbs. However, there are challenges the team must overcome before these vesicles might see clinical use.
“First, we need to develop an effective delivery system to ensure the exosomes remain stable and work properly inside the body,” explained Xinwu. “Additionally, producing enough high-quality exosomes is essential, as each batch must have consistent activity and purity. Extensive clinical trials are also needed to confirm the therapy’s long-term safety and effectiveness for patients.”
Meanwhile, monitoring blood Netrin1 levels could help doctors identify high-risk patients before the condition progresses, enabling early intervention. While Netrin1 shows promise as a diagnostic tool, the team say they are working to confirm its reliability in clinical practice.
“Next steps include conducting larger animal studies to further confirm the effects and safety of Netrin1-enriched exosomes,” said Xinwu. “If these studies show positive results, we plan to initiate preliminary human trials. We’re also working on ways to optimize exosome delivery, ensuring they’re stable in the body and effectively reach the targeted tissues.
“Our ultimate goal is to bring this innovative therapy to the clinic, providing a safe, non-invasive treatment option for diabetic limb ischemia patients.”
Reference: Zhijue Xu, Xing Zhang, Xinwu Lu, et al., Netrin1-Enriched Exosomes From Genetically Modified ADSCs as a Novel Treatment for Diabetic Limb Ischemia, Advanced Healthcare Materials (2024). DOI: 10.1002/adhm.202403521
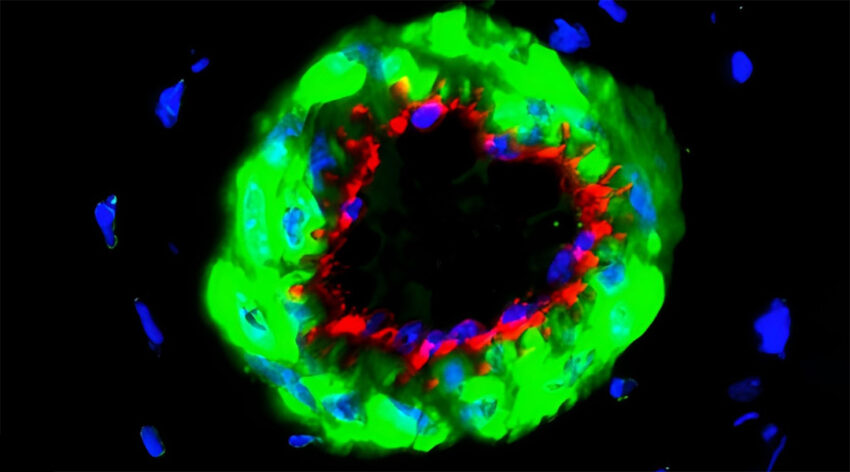
Feature image credit: Zhijue Xu, Xing Zhang, Xinwu Lu, et al