A global study looks into the prevalence of neurological symptoms in patients with COVID-19.
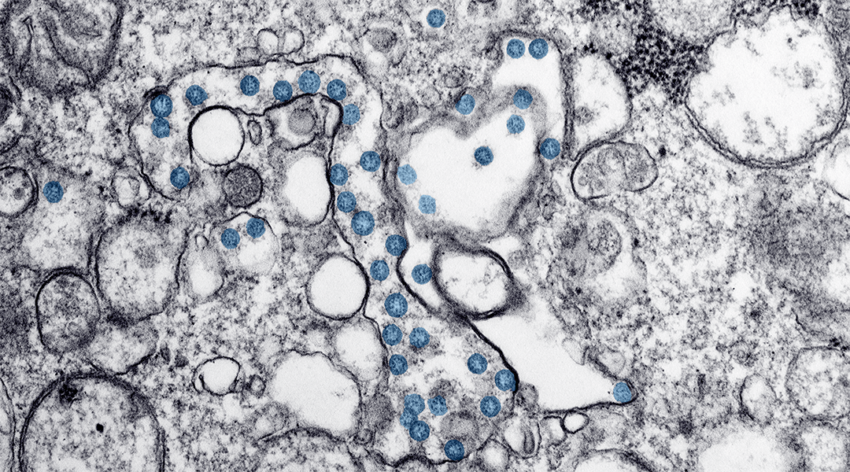
Image credit: CDC
As the situation around the COVID-19 pandemic continues to unfold, researchers are continually learning more about how the underlying virus affects the body, which is important in learning how to treat it while a vaccine is being developed.
The most commonly reported symptoms of COVID-19 to date are difficulty breathing, fever, and cough. However, more and more studies are reporting a range of neurological and neurophysiological complications, which include confusion, stroke, inflammation of the brain and spinal cord, among others.
In one study published this week in The Lancent Neurology, researchers from the University of Liverpool gathered data reporting on the observation of symptoms such as stroke, delirium, and other complications in COVID-19 patients in countries with large outbreaks.
According to the team, both the more innocuous corona-viruses as well as epidemic strains, such as severe acute respiratory syndrome (SARS) caused by SARS-CoV in 2002–2003, and Middle East respiratory syndrome (MERS) by MERS-CoV in 2012, have been associated with occasional disease of the central and peripheral nervous systems.
Their current study analyzed findings from publications around the world, including China, Italy, and the US, which reported neurological complications associated with COVID-19. Data so far suggests that SARS-CoV-2 or related coronaviruses are not highly neurovirulent, unlike other viruses such as the herpes simplex virus, which can cause rampant destruction of neurons. However, the team found that almost 1000 patients in these studies reported a brain, spinal, or nervous disease, which can be considered as a direct effect of the virus or neurological complications that were triggered as a result of infection.
Although neurological complications are rare in SARS, MERS, and COVID-19, the scale of the current pandemic means that even a small proportion could build up to a large number of cases, wrote the authors in their study. This has great significance given the expectation that 50–80% of the world’s population might be infected before herd immunity develops.
As the authors point out, neurological complications, particularly encephalitis and stroke, can cause lifelong disability with associated long-term care needs and potentially large health, social, and economic costs.
Professor Tom Solomon, senior author on the paper and director of the Global COVID-Neuro Network, said in a statement: “Although such patients are being seen everywhere the virus occurs, many of the reports are lacking in detail. We are currently pooling data from individual patients all around the world, so that we can get a more complete picture. Doctors who would like to contribute patients to this analysis can contact us via the Global COVID-Neuro Network website.”
With more patients expected to experience neurological symptoms as a result of SARS-CoV-2 infection, it is important to determine how the virus infects the brain and how healthcare officials and policy makers can prepare for this growing burden.